Maternal mortality remains a pressing issue in the United States, where the rates have alarmingly increased over the past few years. Defined as the death of a woman during pregnancy or within 42 days after childbirth, maternal mortality encompasses a broader spectrum of pregnancy-related deaths than many recognize. With figures reflecting significant disparities among racial and ethnic groups, the maternal health crisis illuminates the urgent need for improved prenatal and postpartum care, particularly in relation to cardiovascular disease in pregnancy. The challenges posed by the U.S. healthcare system and socio-economic factors contribute to these alarming trends, especially given the troubling rise in U.S. pregnancy rates and resultant complications. Addressing this crisis requires immediate collective action to ensure that every individual has access to comprehensive maternal healthcare, thereby reducing preventable deaths.
The issue of maternal mortality, also referred to as pregnancy-associated mortality, highlights the gravity of health outcomes related to childbirth across various demographics. With rising concerns over pregnancy-related deaths, especially in the context of recent public health challenges, the need for systemic reforms in maternity care is emphasized. Disparities in maternal health outcomes underscore a critical maternal health crisis, exacerbated by inadequate postpartum care and rising prevalence of chronic conditions, such as cardiovascular issues among expectant mothers. As the nation grapples with its alarming maternal mortality rates, it is evident that addressing underlying health inequities and expanding support for mothers can pave the way towards enhanced maternal well-being. The pursuit of solutions to this escalating problem has become not only a health imperative but a moral obligation.
Understanding Maternal Mortality in the U.S.
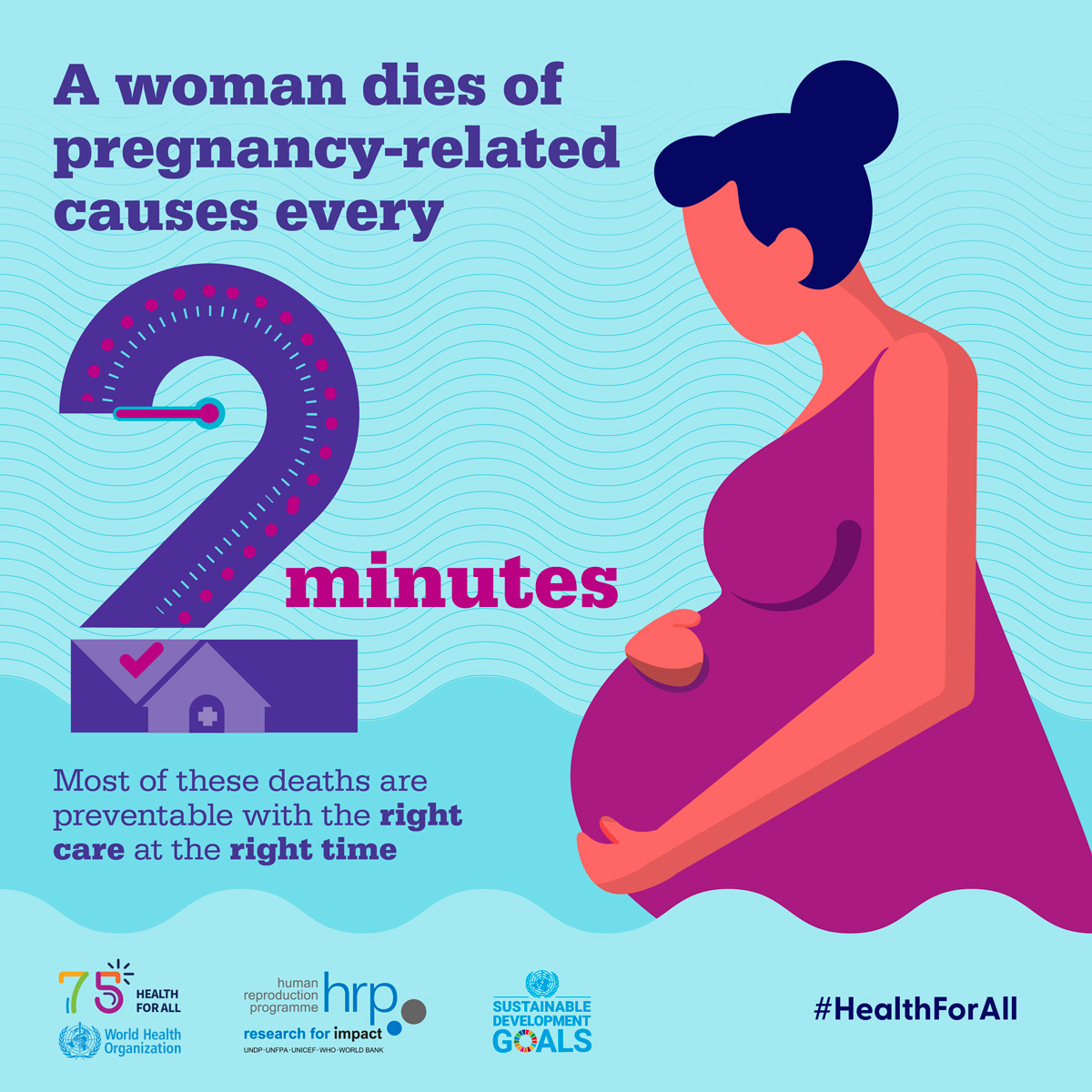
Maternal mortality in the United States remains alarmingly high compared to other high-income countries. According to recent studies, the U.S. leads in maternal mortality rates, with over 80% of pregnancy-related deaths deemed preventable. The persistent rise in these rates from 2018 to 2022 highlights a serious maternal health crisis that demands urgent attention. Disparities in mortality rates across different racial and ethnic groups have further complicated the issue, revealing systemic inequities that have severe implications for maternal health services.
The challenges associated with maternal mortality stem from various factors, including the fragmentation of healthcare, inadequate access to quality prenatal and postpartum care, and socio-economic disparities. These findings underscore the need for a consolidated approach to maternal health, addressing not only immediate care needs but also long-term health concerns in women of reproductive age, particularly those at risk of cardiovascular diseases during and after pregnancy.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
Maternal mortality in the U.S. is primarily caused by cardiovascular disease, which accounts for over 20% of pregnancy-related deaths. Other significant causes include hemorrhage and various complications arising from chronic conditions such as hypertension and pre-eclampsia.
How has maternal mortality changed in the U.S. recently?
Maternal mortality rates in the U.S. have continued to rise, with a notable increase between 2018 and 2022. The rate of pregnancy-related deaths increased from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022, highlighting an ongoing maternal health crisis.
Why do racial disparities in maternal mortality rates exist in the U.S.?
Racial disparities in maternal mortality rates stem from systemic issues such as inequities in healthcare access, discrimination, and varying quality of prenatal and postpartum care across racial groups. For instance, American Indian and Alaska Native women experience the highest mortality rates, nearly four times higher than white women.
What role does postpartum care play in maternal mortality?
Postpartum care is crucial in reducing maternal mortality, as nearly one-third of maternal deaths occur late, between 42 days to one year after childbirth. Improved healthcare systems that extend care beyond the initial six weeks postpartum are essential for addressing the ongoing health needs of mothers.
How does the U.S. maternal mortality rate compare to other high-income countries?
The U.S. leads in maternal mortality rates among high-income countries, primarily due to a fragmented healthcare system and a lack of comprehensive maternal health services. This contributes to preventable pregnancy-related deaths that continue to rise.
What can be done to reduce maternal mortality in the U.S.?
To reduce maternal mortality, investments in public health infrastructure and innovative healthcare solutions are necessary. Improving access to quality care during pregnancy and extending postpartum support is essential to address the ongoing maternal health crisis.
What impact has the COVID-19 pandemic had on maternal mortality rates?
The onset of the COVID-19 pandemic appears to have exacerbated maternal mortality rates, with the sharpest increase occurring in 2021. The ongoing rise in pregnancy-related deaths reflects the need for systemic changes in maternal healthcare.
What are ‘late maternal deaths’ and why are they significant?
Late maternal deaths refer to those occurring between 42 days and one year after childbirth. They are significant because they highlight the need for continuous healthcare support beyond the traditional postpartum period, indicating gaps in maternal health care systems that must be addressed.
How can states improve maternal health outcomes to reduce pregnancy-related deaths?
States can improve maternal health outcomes by analyzing and addressing disparities in care, implementing policies that enhance access to comprehensive maternal services, and investing in education for healthcare providers on the importance of monitoring maternal health well into the postpartum period.
What is the importance of tracking maternal mortality data?
Tracking maternal mortality data is vital for identifying trends, disparities, and systemic issues within maternal healthcare. Accurate data helps inform policy changes and resource allocations aimed at improving maternal health outcomes across different populations.
| Key Point | Details |
|---|---|
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| Rising Maternal Mortality Rate | The U.S. has the highest maternal mortality rate among high-income countries, and it has been rising since 2018. |
| Disparities | Significant disparities exist by race and state, with American Indian and Alaska Native women experiencing the highest rates (106.3/100,000 live births). |
| Leading Causes | Cardiovascular disease was the leading cause of maternal death, with over 20% of deaths attributed to it. |
| Late Maternal Deaths | Nearly a third of maternal deaths occurred between 42 days to 1 year postpartum, which is often not included in traditional definitions. |
| Health System Improvements | A call for better prenatal and extended postpartum care and investment in public health infrastructure is essential to improve maternal health outcomes. |
Summary
Maternal mortality remains a critical issue in the U.S., with the latest findings indicating that the country leads high-income nations in pregnancy-related deaths. Addressing this alarming trend requires urgent improvements in prenatal and postpartum care. It is vital to understand that over 80% of these deaths are preventable, signaling a clear pathway for healthcare improvements. Moreover, the significant disparities across racial and geographic lines highlight the need for tailored interventions. To reduce maternal mortality, a comprehensive approach to healthcare reform is essential, focusing on quality care during and after pregnancy.
Comments are closed, but trackbacks and pingbacks are open.