TIM-3 therapy for Alzheimer’s is emerging as an innovative approach to tackle the challenges posed by this debilitating disease. Recent research has demonstrated how targeting the TIM-3 checkpoint molecule can effectively enhance the brain’s immune response, specifically in combating amyloid plaques associated with Alzheimer’s. By freeing microglia—our brain’s immune cells—to attack these harmful plaques, cognitive improvement in mice has been observed, offering hope for a potential Alzheimer’s new treatment. With many existing cancer therapies focusing on checkpoint molecules, repurposing TIM-3 inhibitors could bridge the gap between cancer research and Alzheimer’s therapy. This groundbreaking work underscores the significance of leveraging the immune system—similarly used in immune system cancer therapy—to address the complexities of Alzheimer’s disease.
The pursuit of innovative treatments for neurodegenerative disorders has led researchers to explore TIM-3 therapy as a promising intervention for Alzheimer’s disease. This novel approach aims to enhance cognitive function by manipulating the brain’s immune response, particularly through the action of microglia. By inhibiting the TIM-3 molecule, these immune cells may clear harmful protein aggregates, thus promoting better memory retention. The proposed therapy represents a potential shift in how Alzheimer’s is treated, moving towards more biologically targeted strategies. This aligns with recent findings that highlight the critical role of immune modulation in neurodegenerative conditions, opening doors to new therapeutic avenues that were previously unexplored.
The Role of TIM-3 in Alzheimer’s Disease
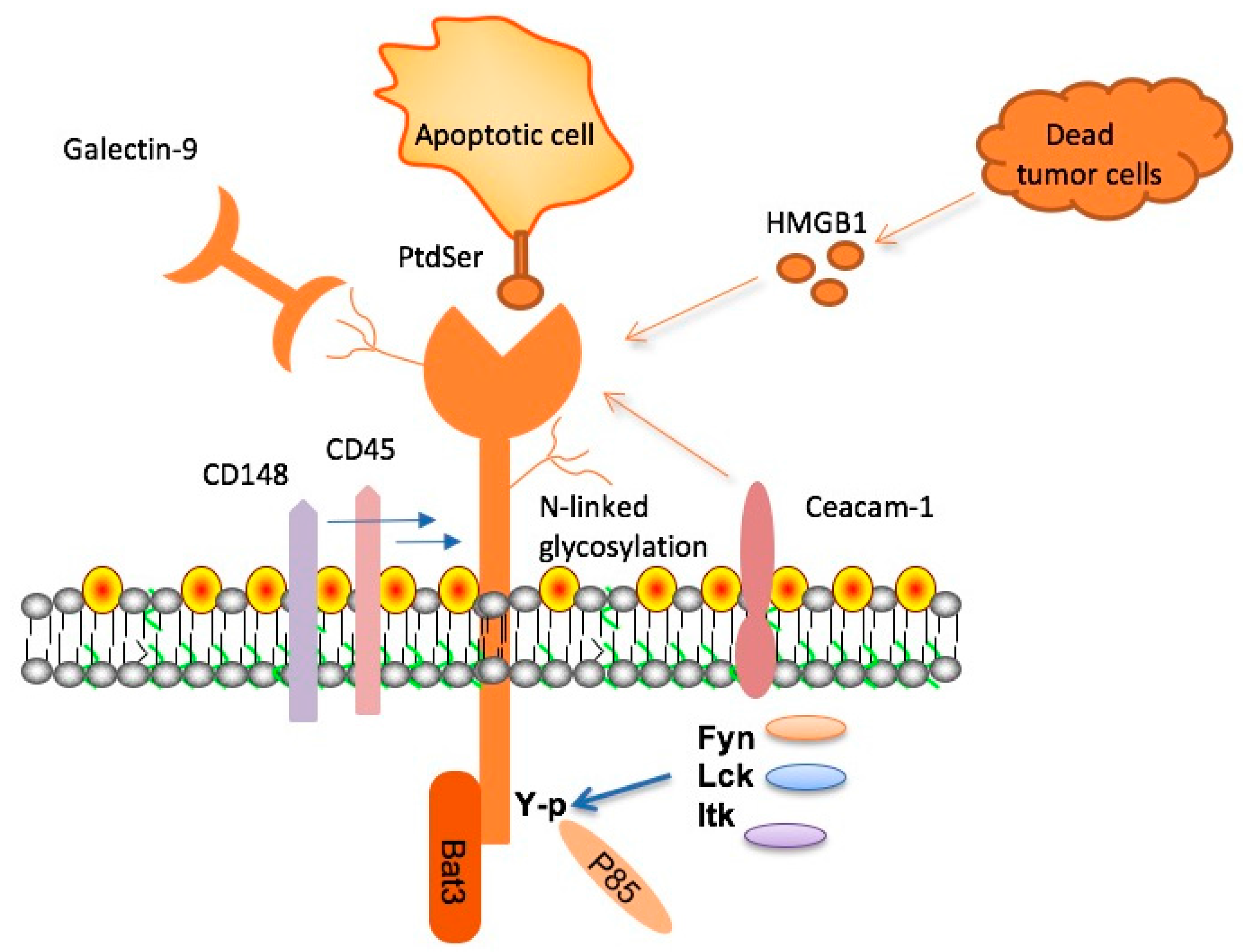
TIM-3, or T-cell immunoglobulin and mucin-domain containing-3, is a checkpoint molecule that plays a dual role in the immune response, particularly in the context of Alzheimer’s disease (AD). Research has revealed that TIM-3 has a heightened expression in the microglia of patients suffering from late-onset Alzheimer’s. This increased expression hampers the microglia’s ability to clear amyloid plaques, which are characteristic of the disease and contribute to cognitive decline. Essentially, TIM-3 inhibits these crucial immune cells from engaging in necessary phagocytic activities, leading to plaque accumulation and worsening symptoms. This mechanism suggests that targeting TIM-3 could restore the function of microglia, enhancing their ability to clear harmful plaques from the brain and potentially reversing cognitive deficits in Alzheimer’s patients.
The interaction between TIM-3 and the immune system’s functionality underscores the complexity of Alzheimer’s pathophysiology. While it is essential for maintaining immune homeostasis and preventing autoimmunity, the maladaptive expression of TIM-3 in aging individuals becomes a substantial roadblock in addressing Alzheimer’s disease. Recent studies, including those involving TIM-3 knockout mice, highlight that deleting this checkpoint molecule can significantly enhance microglial activity. Consequently, these findings open new avenues for developing TIM-3 therapy, which may not only help in plaque clearance but also improve overall cognitive function in affected individuals.
Effects of TIM-3 Therapy in Mice
In preclinical studies, TIM-3 therapy has demonstrated promising results in improving cognition among mouse models of Alzheimer’s disease. By genetically altering mice to lack the HAVCR2 gene, which encodes for the TIM-3 molecule, researchers observed a remarkable increase in the clearance of amyloid plaques by microglia. This process not only reduced plaque burden but also altered the physical properties of the plaques, making them less toxic. Following these interventions, the cognitive behaviors of these mice improved significantly; they began to navigate mazes and hide in response to potential threats better, indicating a restoration of memory functions.
These findings mark a significant step forward in the quest for effective Alzheimer’s treatments. The cognitive improvements seen in TIM-3 knockout mice suggest that therapies aimed at inhibiting this checkpoint molecule could potentially reverse some of the degenerative processes associated with dementia. If similar results can be replicated in human trials, TIM-3 therapy could revolutionize the treatment of Alzheimer’s, shifting focus from merely slowing disease progression to actual cognitive restoration.
Implications of Checkpoint Molecules in Alzheimer’s Treatment
The concept of utilizing checkpoint molecules like TIM-3 in the treatment of Alzheimer’s disease signifies a paradigm shift in how researchers understand and approach neurodegenerative diseases. Traditionally, Alzheimer’s treatments have targeted the reduction of amyloid beta production, leading to minor improvements in cognitive function. In contrast, TIM-3 therapy aims to manipulate the immune system’s natural ability to clear accumulations in the brain, potentially offering a more holistic treatment approach. By repurposing existing anti-TIM-3 antibodies developed for cancer therapy, researchers are exploring innovative strategies to harness the body’s own immune response against neurodegeneration.
These research advancements highlight the intimate connection between immune function and Alzheimer’s pathology. Harnessing immune checkpoints could not only lead to better therapeutic outcomes but also provide insights into the underlying mechanisms of the disease. As scientists continue to investigate the interplay between TIM-3, microglia, and amyloid plaques, a clearer understanding of Alzheimer’s pathophysiology will emerge, allowing for the development of targeted immunotherapies that could dramatically shift the current treatment landscape.
Potential Obstacles in Developing TIM-3 Therapy
While the potential of TIM-3 therapy for Alzheimer’s disease is promising, several challenges remain in the pathway toward clinical application. First, it is crucial to ensure that targeting TIM-3 does not inadvertently trigger autoimmunity or other adverse immune responses. Given that checkpoint molecules like TIM-3 play a protective role in regulating immune activity, any therapy that disrupts this balance needs to be meticulously designed and tested to avoid potential complications. Furthermore, rigorous clinical trials will be essential to establish the efficacy and safety of TIM-3 inhibition in human subjects.
Additionally, the unique characteristics of Alzheimer’s pathology in humans compared to animal models may pose another hurdle. While the initial studies in mice have shown significant cognitive improvements, translating these findings to humans requires careful consideration of genetic and environmental variables that affect disease progression. Future research will need to determine the most effective formulations for TIM-3-targeting agents and their administration routes, paving the way for their safe integration into existing Alzheimer’s treatment protocols.
Current Research Directions for TIM-3 in Neurodegeneration
As research progresses, the focus on TIM-3 as a therapeutic target for Alzheimer’s disease has intensified, leading to the exploration of various drug formulations designed to inhibit this checkpoint molecule. Current studies are increasingly looking at humanized mouse models that incorporate the human TIM-3 gene, allowing for the evaluation of candidate antibodies tailored for human physiology. These advancements mark a critical step toward validating the TIM-3 therapy’s potential effectiveness in clearing amyloid plaques and restoring cognitive functions in Alzheimer’s patients.
Collaboration between leading research institutions and pharmaceutical companies is crucial to advancing this field. By sharing findings and pooling resources, researchers can accelerate the pace of discovery in developing TIM-3 therapies. The integration of advanced technologies such as monoclonal antibodies and small molecules could further refine therapeutic strategies aimed at modulating immune responses in the brain. As this research continues to unfold, it holds the promise of not only treating Alzheimer’s disease but also offering insights that could revolutionize our understanding of other neurodegenerative conditions.
Comparative Analysis of Alzheimer’s Treatment Approaches
When considering the diverse landscape of Alzheimer’s treatments, TIM-3 therapy presents a novel approach that contrasts with traditional drug regimens focusing solely on symptomatic relief. Conventional treatments primarily target neurotransmitter levels to manage symptoms like memory loss and cognitive decline, but they often fall short of addressing the underlying pathophysiological processes. In comparison, TIM-3 therapy aims at enhancing the brain’s immune activity by promoting plaque clearance, potentially leading to more substantive cognitive improvements. This shift signifies a move from palliation to a more proactive restoration of brain function.
Moreover, the exploration of TIM-3 alongside existing therapies could yield synergistic effects, enhancing the overall efficacy of treatment plans. By integrating TIM-3 inhibitors with standard Alzheimer’s medications, healthcare providers may be able to offer patients a more comprehensive strategy for managing their condition. This potential for combinatory treatments underscores the significance of understanding the multifactorial nature of Alzheimer’s disease, opening up pathways for research and innovation that may ultimately lead to breakthroughs in cognitive health.
Patient Perspectives on TIM-3 Therapy for Alzheimer’s
In light of emerging research on TIM-3 therapy, it is crucial to consider the experiences and opinions of Alzheimer’s patients and their families. Many patients seek treatments that go beyond merely alleviating symptoms, aspiring for therapies that can restore cognitive functions and improve quality of life. As studies on TIM-3 therapy progress into human clinical trials, the expectations and hopes of patients and caregivers play an essential role in shaping the discourse around new therapeutic options. Engaging patient communities in this research is vital for understanding their needs and determining the most impactful treatment strategies.
Furthermore, as families await new treatment options like TIM-3 therapy to reach the market, they often express concerns regarding safety and effectiveness. Transparency in research findings, coupled with clear communication from healthcare providers, will be crucial in fostering trust and understanding. As evidence mounts regarding the efficacy of TIM-3 in mouse models, it’s important for researchers to actively involve patients in discussions about potential outcomes and back up expectations with solid data. This collaborative approach will ensure that advancements in Alzheimer’s therapy resonate strongly with patient needs and aspirations.
Future Directions for Alzheimer’s Therapeutics
The promising results associated with TIM-3 therapy for Alzheimer’s not only illustrate the potential for changing therapeutic landscapes but also highlight the need for ongoing research. Future directions will likely involve refining TIM-3 inhibitors and assessing their long-term effects on cognitive function and overall brain health in humans. Additionally, researchers must explore the applicability of TIM-3 interventions in various stages of Alzheimer’s, determining whether early intervention could yield more robust protective effects against cognitive decline.
Research initiatives should also focus on the role of TIM-3 in conjunction with other biomarkers related to Alzheimer’s disease, which may provide a more panoramic understanding of the condition. By combining the study of immune checkpoints with other molecular targets, scientists may develop comprehensive therapies that not only clear plaques but also rejuvenate neurological pathways. This multidisciplinary approach could revolutionize Alzheimer’s treatment, steering efforts toward more effective prevention strategies and paving the way for a healthier aging population.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 checkpoint molecule to enhance immune response in the brain. Research shows that deleting TIM-3 expression allows microglia, the brain’s immune cells, to clear amyloid plaques, potentially improving cognition and memory in Alzheimer’s models.
How does TIM-3 checkpoint molecule relate to Alzheimer’s new treatment options?
The TIM-3 checkpoint molecule plays a critical role in Alzheimer’s disease by inhibiting microglial activity. New treatments aim to block TIM-3, enabling microglia to effectively attack harmful amyloid plaques and restore cognitive functions in Alzheimer’s patients.
What evidence supports TIM-3 therapy’s effectiveness for improving cognition in Alzheimer’s patients?
Studies on mice genetically modified to lack TIM-3 show significant reductions in plaque accumulation and improvements in cognitive tasks, indicating that TIM-3 therapy could be a viable approach to enhance cognitive functions in Alzheimer’s patients.
Can TIM-3 therapy help microglia clear amyloid plaques in Alzheimer’s disease?
Yes, TIM-3 therapy helps microglia clear amyloid plaques by inhibiting the TIM-3 checkpoint, which normally suppresses microglial activity. With TIM-3 blocked, microglia can effectively remove plaques that contribute to Alzheimer’s pathology.
What potential does TIM-3 checkpoint therapy hold for Alzheimer’s treatment?
TIM-3 checkpoint therapy holds significant potential for Alzheimer’s treatment by offering a targeted approach to reduce amyloid plaque accumulation, as demonstrated in animal models that showed improved memory and cognitive performance following TIM-3 inhibition.
In what way does TIM-3 therapy differ from traditional Alzheimer’s treatments?
Unlike traditional Alzheimer’s treatments that focus on symptomatic relief, TIM-3 therapy aims to modify the disease process by enhancing the brain’s immune response to eliminate plaques, potentially leading to cognitive improvement.
What role do microglia play in Alzheimer’s disease concerning TIM-3 therapy?
Microglia are the primary immune cells in the brain and are essential for clearing amyloid plaques. TIM-3 therapy enhances microglial activity by inhibiting the TIM-3 molecule, which allows these cells to attack and clear the damaging plaques associated with Alzheimer’s.
What are the next steps for TIM-3 therapy research in Alzheimer’s disease?
The next steps include evaluating the efficacy of human anti-TIM-3 antibodies in preclinical models of Alzheimer’s disease, particularly focusing on their ability to prevent plaque formation and enhance cognitive function in affected mice.
How does TIM-3 therapy compare to other Alzheimer’s treatment strategies?
TIM-3 therapy offers a novel approach, contrasting with other strategies that primarily target amyloid levels without addressing underlying immune mechanisms. By promoting microglial activity, TIM-3 therapy could lead to more effective cognitive improvement outcomes.
What challenges do researchers face when developing TIM-3 therapy for Alzheimer’s?
Researchers face challenges such as ensuring the specificity of TIM-3 inhibitors to prevent unwanted immune responses, optimizing delivery methods to the brain, and demonstrating significant cognitive improvements in human trials similar to those observed in animal models.
| Key Point | Details |
|---|---|
| TIM-3 Therapy | Refers to a potential treatment strategy using TIM-3 checkpoint inhibition to enhance microglial activity against Alzheimer’s plaques. |
| Background | 90-95% of Alzheimer’s cases are late-onset, linked to TIM-3 as a genetic risk factor. |
| Microglia Role | Microglia are brain immune cells that clear amyloid plaques; they become inhibited by high levels of TIM-3. |
| Study Findings | Deletion of TIM-3 in lab mice enhanced plaque clearance and improved cognitive function. |
| Future Therapy | Potential human therapy could involve anti-TIM-3 antibodies or small molecules to block TIM-3. |
| Research Duration | The study process took five years, involving collaboration between multiple scientists. |
| Next Steps | Further testing of human anti-TIM-3 in mouse models to see if it can prevent plaque formation. |
Summary
TIM-3 therapy for Alzheimer’s represents a promising new approach that could leverage immune system mechanisms previously used to combat cancer. The findings indicate that blocking TIM-3 has the potential to enhance the brain’s ability to clear harmful amyloid plaques, which are a hallmark of Alzheimer’s disease. Future studies may lead to effective treatments that restore cognitive function, offering hope to millions affected by this devastating condition.
Comments are closed, but trackbacks and pingbacks are open.